Services
 Endovenous laser ablation (EVLA) treats major varicose veins previously treated by stripping surgery. We use the latest highly advanced and skilled method to treat varicose veins. It’s a day care procedure with quick recovery, under regional anaesthesia, no obvious scars, no stiches (suture), no blood loss with ultrasound guidance, a laser fibre is placed into the abnormal vein through a tiny incision. This produces a reaction in the vein wall along the treated section, resulting in collapse and sclerosis of the vein wall with minimal discomfort. The success of EVLA treatment is between 95-98%, with far fewer complications than surgery. With the addition of EVLA to ultrasound guided sclerotherapy is performed on case basis. The common tendency of individuals is to neglect the signs & symptoms of varicose veins and have their legs covered, yet consult the doctor only when it gets very troublesome. Appropriate early treatment will prevent from many worries like discoloured dark skin, non-healing wounds & ulcers, crampy leg pain, itching and prominent abnormal looking veins.
Endovenous laser ablation (EVLA) treats major varicose veins previously treated by stripping surgery. We use the latest highly advanced and skilled method to treat varicose veins. It’s a day care procedure with quick recovery, under regional anaesthesia, no obvious scars, no stiches (suture), no blood loss with ultrasound guidance, a laser fibre is placed into the abnormal vein through a tiny incision. This produces a reaction in the vein wall along the treated section, resulting in collapse and sclerosis of the vein wall with minimal discomfort. The success of EVLA treatment is between 95-98%, with far fewer complications than surgery. With the addition of EVLA to ultrasound guided sclerotherapy is performed on case basis. The common tendency of individuals is to neglect the signs & symptoms of varicose veins and have their legs covered, yet consult the doctor only when it gets very troublesome. Appropriate early treatment will prevent from many worries like discoloured dark skin, non-healing wounds & ulcers, crampy leg pain, itching and prominent abnormal looking veins.
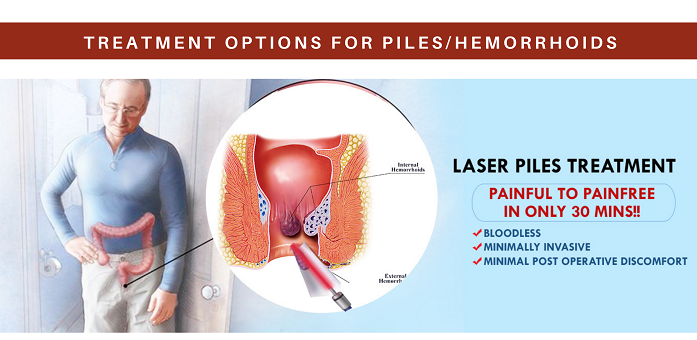
The laser is the latest modality for fissures, fistulas, and piles. It is a daycare procedure that offers several advantages over traditional surgery.
- Less operation time
- Discharge within a few hours
- Go back to a normal routine within a day or two
- Great surgical precision
- Faster recovery
- Significantly less post-operative pain
- Less recurrence rates
- Anal sphincter is well preserved (no chances of incontinence/ fecal leak)
Piles
Laser Haemorrhoidectomy
Laser cauterization is a technique in which the surgeon uses a narrow beam of the laser to focus only on hemorrhoid and not damage the nearby tissues. It is a safe procedure with minimal bleeding and quick healing time. The controlled emission of laser energy reaches the submucosa zone, causing the haemorrhoidal mass to shrink. Fibrotic reconstruction generates new connective tissue, ensuring the mucosa adheres to the underlying tissue preventing the recurrence of prolapse.
Fistulas
FILAC technique (Fistula – Tract Laser Closure)
It is a minimally invasive and sphincter-preserving technique used in treating anorectal fistula. The affected tissue (epithelialized path) is destroyed and sealed using laser emission radially 360° in a controlled manner. Laser energy is delivered into the anal fistula tract which induces destruction of the fistula epithelium and simultaneous obliteration of the remaining fistula tract by a shrinkage effect. The epithelialized tissue is being destroyed in a controlled way and the fistula tract collapses to a very high degree. Using radial fiber gives good control to the operator and also allows use in the convoluted track.
Fissure
The laser fissure procedure is done under local anesthesia. It doesn’t require hospitalization of a patient. By the use of laser, pathological tissue of anal fissure is vaporized. The laser removal of the fissure has great efficiency rate. It is the most modern technique to treat a fissure. The laser surgery is the perfect alternative for the other methods.
Pilonidal Sinus
Contrary to the conventional methods, the laser treats pilonidal sinuses in depth. It is literally a non-invasive, completely painless and very therapeutic effect of laser that contributes noticeably to the spectacular healing of pilonidal sinus disease. Laser removes the inflamed structures and the sinuses. The removal of pilonidal sinuses with this laser surgical technique takes approximately 30 minutes in most cases. When we laser the sinus tracts, collateral damage is minimal. The healing process is thus quicker, easier and mostly without any pain. Chances of recurrences are minimal.
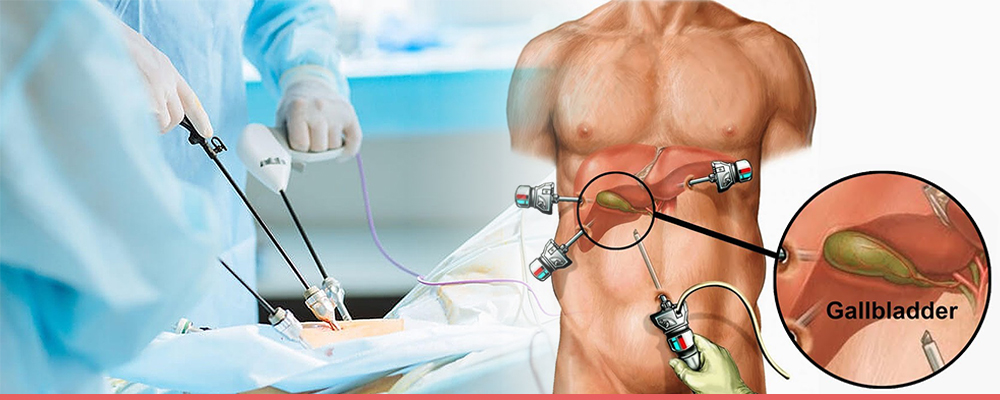
Laparoscopic cholecystectomy takes about an hour or two. A surgeon will make a few small incisions in your abdomen. The surgeon will insert thin, hollow tubes into those incisions. The surgical team will then place a laparoscope and other surgical tools into the tubes.
Surgical team may pump carbon dioxide into your abdomen. This step inflates the surgical area and makes it easier to see inside. Using the special tools, the surgeon will detach the gallbladder from the rest of the body and remove it. The team will then close the incisions with stitches, surgical clips or surgical glue.
If any complications occur during laparoscopic cholecystectomy, the surgeon may decide to use an open cholecystectomy instead. That procedure involves a larger incision.
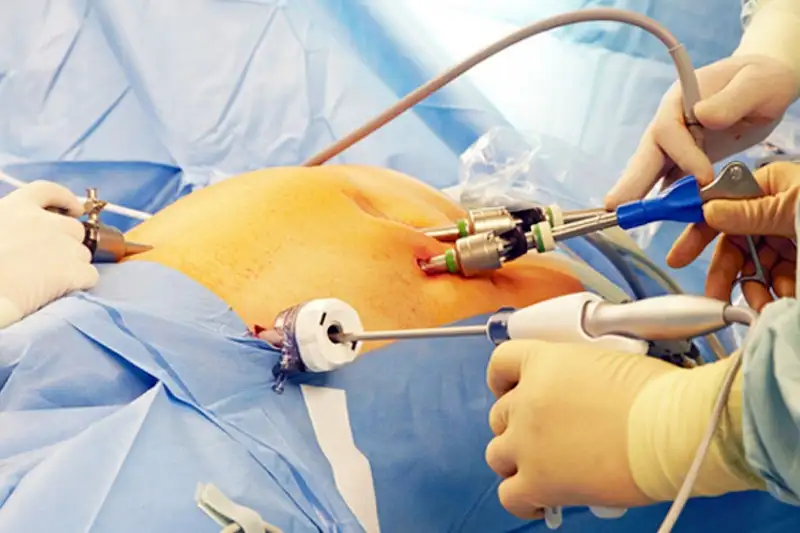
This method is minimally invasive. That means 1 to 3 tiny cuts are made. A long, thin tube called a laparoscope is put into one of the incisions. It has a tiny video camera and surgical tools. Surgeon looks at a TV monitor to see inside your abdomen and guide the tools. The appendix is removed through one of the incisions.
During a laparoscopic surgery, your provider may decide that an open appendectomy is needed.
If your appendix has burst and infection has spread, you may need an open appendectomy.
A laparoscopic appendectomy may cause less pain and scarring than an open appendectomy. For either type of surgery, the scar is often hard to see once it has healed.
Both types of surgery have low risk of complications. A laparoscopic appendectomy has a shorter hospital stay, shorter recovery time, and lower infection rates.
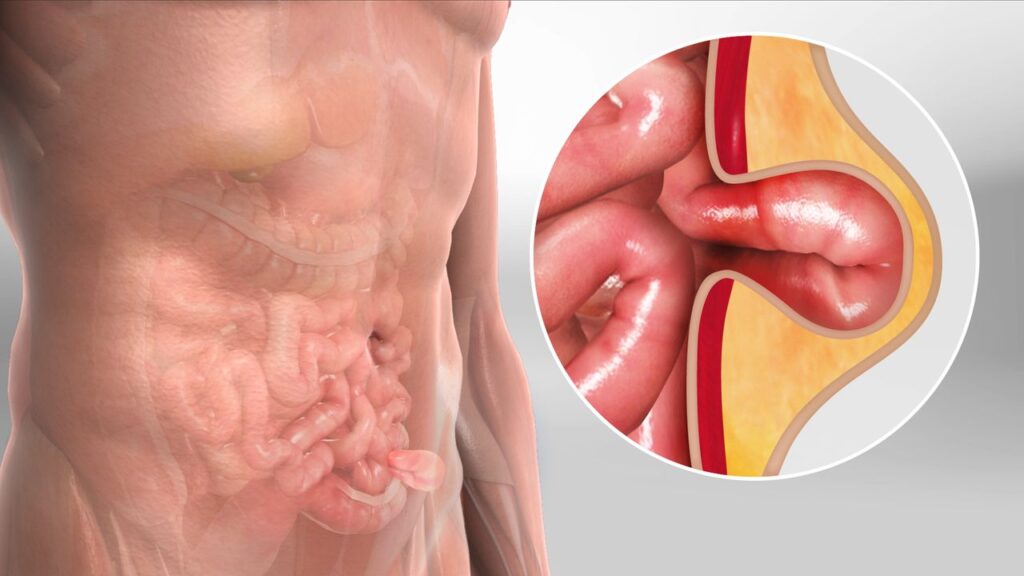
Laparoscopic (minimally invasive) hernia repair uses a laparoscope, a thin, telescope-like instrument that is inserted through a small incision at the umbilicus (belly button). This procedure is usually performed under general anesthesia, so before the surgery, you will have an evaluation of your general state of health, including a history, physical exam (and possibly lab work) and an electrocardiogram (EKG).
You will not feel pain during this surgery. The laparoscope is connected to a tiny video camera, smaller than a dime, that projects an “inside view” of your body onto television screens in the operating room.
The abdomen is inflated with a harmless gas (carbon dioxide), which creates space to allow your doctor to view your internal structures. The peritoneum (the inner lining of the abdomen) is cut to expose the weakness in the abdominal wall. Mesh is placed on the inside to cover the defects in the abdominal wall and strengthen the tissue.
After the procedure is completed, the small abdominal incisions are closed with a stitch or two or with surgical tape. Within a few months, the incisions are barely visible.
Benefits of laparoscopic hernia surgery include three tiny scars rather than one larger incision, less pain after surgery, a quicker return to work and a shorter recovery time (days instead of weeks).
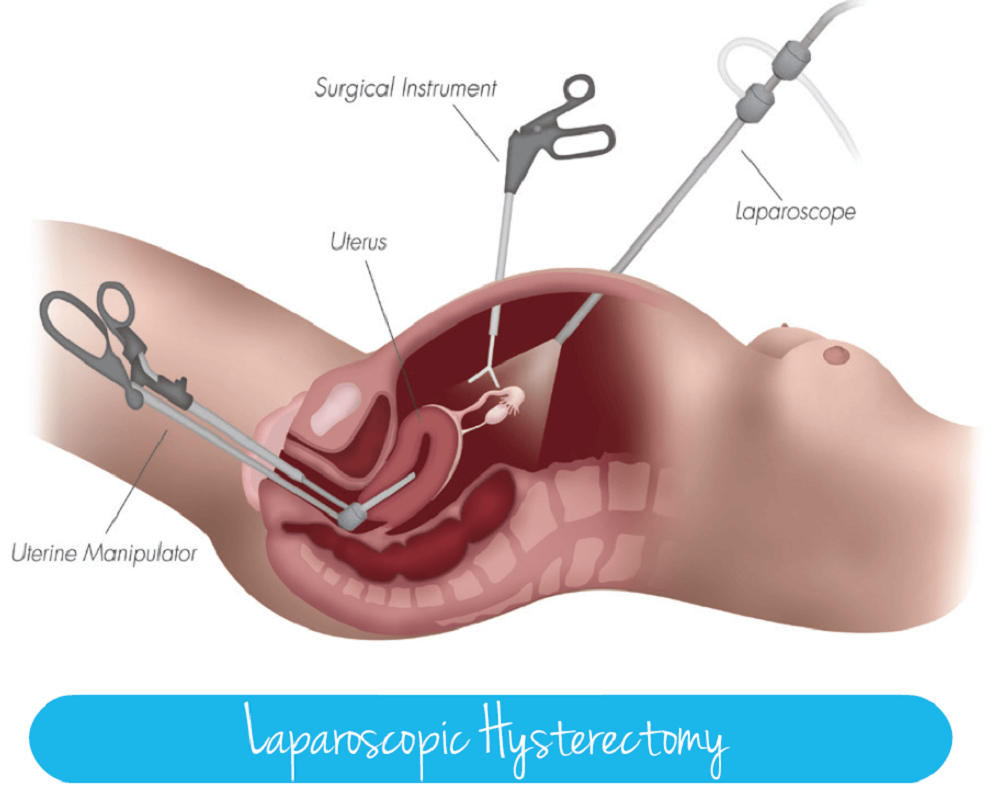
Laparoscopic hysterectomy is a surgical procedure for the removal of uterus. In this technique, the uterus is separated from inside of the body and removed in small pieces through small incisions or through vagina. A hysterectomy is a major surgical procedure and has both psychological and physical consequences.
This allows the surgeon to see your internal organs. Instruments are then inserted through other small incisions in your abdomen or vagina to remove your womb, cervix and any other parts of your reproductive system. Laparoscopic hysterectomies are usually carried out under general anaesthetic.
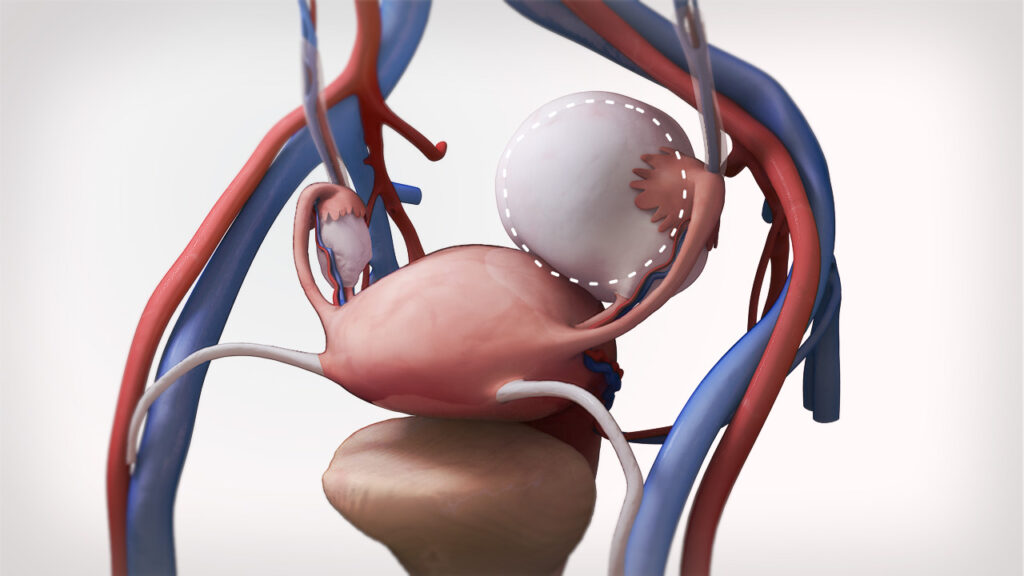
An ovarian cystectomy is surgery to remove a cyst from your ovary. Laparoscopic surgery is a minimally invasive surgery technique that only uses a few small incisions in your lower abdomen.
After the ovarian cyst removal, you may feel pain in your tummy, which should improve in a few days. After the ovarian cyst removal, you may feel pain in your tummy, which should improve in a few days. The time for recovery after a laparoscopic ovarian cystectomy may be different for everyone.
Most patients are fully recovered in four to six weeks. If a patient has a physically demanding job that requires lifting or pushing heavy objects, check with the doctor before returning to work.
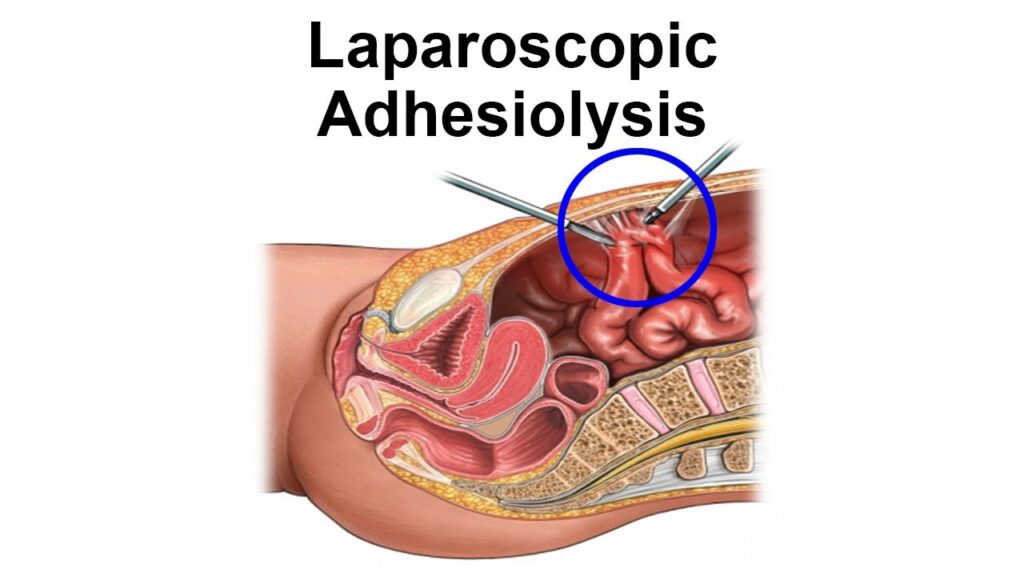
Abdominal adhesions often don’t cause noticeable symptoms. Adhesions often go undiagnosed because they aren’t visible with current imaging methods.
However, for some people, they can cause chronic pain and abnormal bowel movements.
If your adhesions are causing problems, laparoscopic adhesiolysis can remove them. It’s a minimally invasive procedure. With laparoscopic surgery, your surgeon will make a small incision in your abdomen and use a laparoscope to locate the adhesion.
A laparoscope is a long thin tube that contains a camera and light. It’s inserted into the incision and helps your surgeon find the adhesions to remove them.
Laparoscopic adhesiolysis may be used to treat the following conditions:
Intestinal blockages
Adhesions can cause problems with digestion and even block the intestines. The adhesions can pinch off part of the intestines and cause a bowel obstruction. The obstruction may cause:
- nausea
- vomiting
- an inability to pass gas or stool
Infertility
Adhesions can cause female reproductive problems by obstructing the ovaries or fallopian tubes.
They can also cause painful intercourse for some people. If your doctor suspects adhesions are causing your reproductive issues, they may recommend surgery to remove them.
Pain
Adhesions can sometimes cause pain, especially if they’re blocking the bowels. If you have abdominal adhesions, you may also experience the following symptoms along with your pain:
- nausea or vomiting
- swelling around your abdomen
- dehydration
- cramps
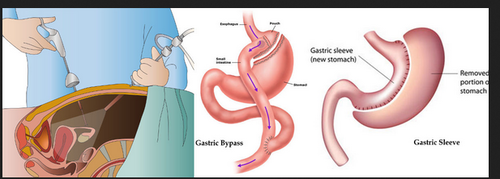
Gastrointestinal surgery is a treatment for diseases of the parts of the body involved in digestion. This includes the esophagus (ee-sof-uh-gus), stomach, small intestine, large intestine, and rectum. It also includes the liver, gallbladder, and pancreas.
Surgery may be used to remove a cancerous or noncancerous growth or damaged part of the body, such as the intestine. It may also be used to repair a problem like a hernia (a hole or weak spot in the wall of the abdomen). Minor surgical procedures are used to screen and diagnose problems of the digestive system.
Below are gastrointestinal conditions that may be treated with surgery:
- Appendicitis. When the appendix becomes infected and inflamed, it may be removed (appendectomy).
- Colon cancer and other gastrointestinal cancers. Surgery is done to remove cancerous tumors in the digestive system and parts of the digestive system that have cancer. For example, a surgeon may remove a tumor as well as part of the pancreas, liver, or intestine with cancer.
- Diverticular disease. A diverticulum is a small pouch or pocket in the colon (large intestine). Researchers are not sure why these develop. Sometimes they can become inflamed and cause pain (diverticulitis). This is often managed without surgery. If someone has a lot of diverticula that often become inflamed, the doctor may recommend bowel resection surgery to remove that part of the intestine.
- Gallbladder disease. When there is a problem with the gallbladder — usually gallstones — the gallbladder can be removed. Surgery to remove the gallbladder is also called a cholecystectomy (koh-luh-si-stek-tuh-mee).
- Gastroesophageal reflux disease (GERD) and hiatal hernias. GERD, or acid reflux is when the acid from the stomach backs up into the esophagus (food pipe) and causes heartburn. Sometimes it happens because of a hiatal hernia. This is when the stomach pushes through the diaphragm, a muscle that separates the chest from the abdomen. A surgeon can do a surgery called fundoplication (fun-doh-pluh-cay-shun) to fix it. The surgeon will fix the hernia if there is one and then wrap the top of the stomach around the bottom of the esophagus to strengthen the sphincter, which keeps acid out.
- Hernia. A hernia is when a part of the body (like the intestine) comes through a hole or weak spot in the wall of muscle or connective tissue that’s supposed to protect it (like the abdomen). It doesn’t come through the skin, but a bulge may be felt under the skin that’s not supposed to be there. It can also be painful. Gastrointestinal surgeons can repair the hole or weak spot.
- Inflammatory bowel disease (Crohn’s disease and ulcerative colitis). With inflammatory bowel disease, the immune system attacks the intestines and causes pain and inflammation. This can lead to damage in the intestine. Sometimes the damaged parts are removed and the healthy parts are reconnected. This is called bowel resection.
- Rectal prolapse. Surgery is used to treat rectal prolapse, a condition in which part of the intestine comes through the anus.
- Weight loss. Different types of bariatric surgery (for example, gastric bypass) may be done to treat obesity. This surgery is usually done by a specialist in bariatric surgery.
A surgical procedure called an endoscopy is used to screen and diagnose problems of the digestive system. The doctor puts a long, thin tube with a tiny camera into the body to see inside. If the problem is with the stomach or esophagus, the doctor puts the scope through the esophagus. To check for colon cancer or other problems of the intestines, the doctor puts the scope through the anus into the intestine.
What are the benefits?
Surgery to remove a tumor or diseased body part, or repair damage, can be lifesaving. Surgery can also improve the quality of life for someone who has not benefited from other treatments, like medicine or diet changes.
Colonoscopy is a minor surgical procedure with big benefits: it can catch colon cancer early enough to cure it. It’s important to get the recommended colon cancer screening.

An upper GI endoscopy is done by a gastroenterologist, who has special training. An upper GI endoscopy can be done in a hospital or an outpatient office. Your doctor will look at the inside of your esophagus — the tube that links your stomach and your mouth — your stomach and the start of your small intestine.
An upper GI endoscopy can be helpful in finding health problems or figuring out the reason you are having certain symptoms, like trouble or pain when swallowing, pain in the stomach, or bleeding. In many cases, an upper GI endoscopy is a better test than X-rays, since the doctor is able to see more clearly.
An upper GI endoscopy uses a long, thin (about the width of your little finger), flexible tube with a tiny camera on the end, called an endoscope. This tube and camera gives your doctor a clear view inside your body.
What’s it like to have an endoscopy?
You will be given medicine to block pain and make you feel sleepy during this test, so you won’t feel or remember much.
During an upper GI endoscopy, the doctor may take a biopsy (small piece of tissue to look at under the microscope). You won’t feel this.
Sometimes, if certain problems are found during the test, tools can be passed through the tube to fix them.
Your gastroenterologist will use the upper GI endoscopy to look for health issues and take tissues samples to find health problems, such as:
- Gastroesophageal reflux disease (GERD).
- Ulcers.
- Cancer or a tumor.
- Swelling.
- Celiac disease.
- Low iron.
Nutritional deficiencies.
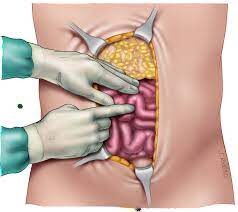
Exploratory laparotomy is an abdominal surgery that doctors sometimes use to diagnose abdominal issues. It is usually recommended when other testing did not diagnose or fully resolve an issue.
Reasons to perform this surgery include:
- Abdominal trauma (for example, from an accident)
- Unexplained bleeding
- Severe pain
- Unexplained pain
- Cancer with undetermined spread
What Do Doctors Do During an Exploratory Laparotomy?
During this surgery, doctors may explore your organs to find the cause of pain or bleeding. The organs they may examine include your:
- Liver
- Kidneys
- Stomach
- Spleen
- Pancreas
- Intestines (both small and large)
- Reproductive organs like your uterus, fallopian tubes, or ovaries
- Appendix
- Blood vessels
- Membranes
- Lymph nodes
During the surgery, depending on what they find, your doctor may take samples or biopsies to send to a lab for testing. If they find the cause of the problem, they may perform surgery to fix it during the exploratory laparotomy.
Conditions that may be discovered during this surgery include:
- Cancer
- Endometriosis
- Infection
- Scar tissue
- Pancreatitis
- Gallstones
- Perforation of the intestines
- Ectopic pregnancy
How to Prepare For an Exploratory Laparotomy
This surgery is sometimes done in emergency situations, like after an accident. If that is the case, there is not much you can do to prepare for it. However, if it is a scheduled surgery:
- Quit smoking a few weeks before the surgery.
- Make sure all other health conditions are well-managed before surgery.
- Tell your doctor about any other supplements, prescriptions, and over-the-counter medications you are taking.
- Be honest with your doctor about your drinking habits.
- Tell your doctor about any possibility of pregnancy.
The week before surgery. In the week before the surgery, your doctor may advise you to stop taking certain kinds of medications. Make sure to clarify which ones you should still take. You should also prepare your home for when you come back from the hospital and make arrangements for any people you will have helping you while you recover.
The day of surgery. Follow your doctor’s instructions about when to stop eating and drinking before your surgery. If you do have to take any medications, take them with a small sip of water to avoid drinking too much liquid. Make sure to get to the hospital on time to keep things running on schedule.
How to Recover From an Exploratory Laparotomy
In general, recovery from an exploratory laparotomy takes 4 to 6 weeks

A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland. In general surgery, endocrine or head and neck surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland or goiter.
A thyroidectomy is a treatment for a variety of diseases, disorders and conditions of the thyroid gland. A thyroidectomy is a common but major surgery with serious risks and potential complications. You may have less invasive treatment options.
Most people take 1 to 2 weeks off to recover. You should not drive for at least a week. There are no other restrictions. Depending on the amount of thyroid tissue that was removed and the reason for your surgery, you may be placed on thyroid hormone.
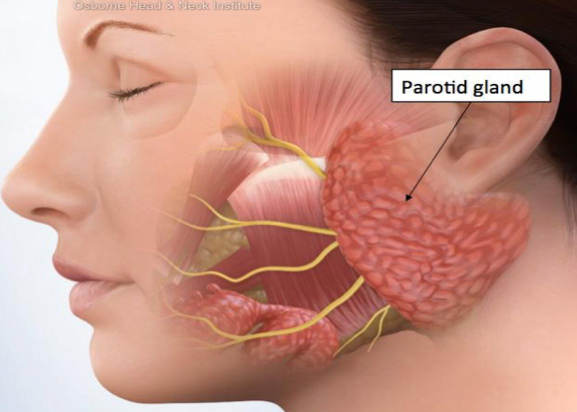
The parotid is a large salivary gland near the ear. It helps produce and control the release of saliva. There’s one on each side of your face. The facial nerves pass through each parotid gland. This nerve controls the muscles on that side of the face. If a tumor forms in the parotid gland, it can press on the facial nerve, causing discomfort and pain. Part or all of one side of the face may be weak or paralyzed. To treat a parotid tumor, part or all of the gland is removed. The amount of the gland removed depends on how much of it is affected. Your doctor may not know how much needs to be taken out until surgery is done. This surgery is called parotidectomy.
During this surgery, steps are taken to protect the facial nerve. This may include using a device called a facial nerve monitor to sense activity in and around the nerve. This helps to map the exact location of the nerve, so the healthcare provider can avoid touching it during surgery. But in some cases, all of the nerve can’t be completely protected. The facial nerve helps you move your lips, close your eye on that side, and wrinkle your nose. You and your healthcare provider will discuss whether your facial nerve is likely to be affected by the surgery, what changes you might have, and what your choices are.
Getting ready for surgery
Get ready for the procedure as you have been instructed. Be sure to tell your healthcare provider about all medicines you take. This includes over-the-counter medicines. It also includes herbs, vitamins, and other supplements. You may need to stop taking some or all of them before surgery. Also, follow any directions you’re given for not eating or drinking before surgery.
The day of surgery
The surgery takes 3 to 5 hours.
After the surgery
You will be taken to a recovery room to wake up from the anesthesia. You may feel sleepy and nauseated at first. You will be given medicine to control pain. You may then be taken to a hospital room to stay for a day or so. Once you are ready to go home, you will be released to an adult family member or friend. Have someone stay with you for a few days to help care for you as your healing begins. If you’re sent home with a drain, you will be shown how to care for it.
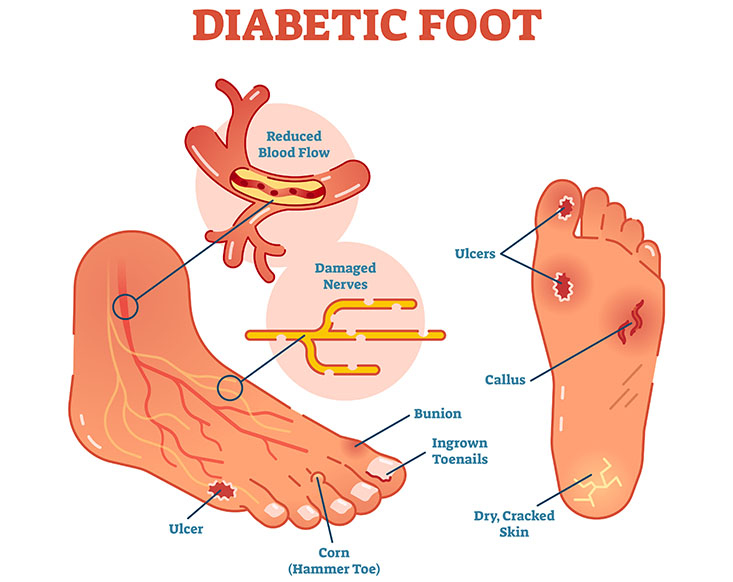
Diabetic foot is one of the feared complications of diabetes.
Chronic high blood sugar leads to blood vessel damage. This includes blood vessels that provide the nerves in your toes, feet, and legs with oxygen and nutrients.
Having uncontrolled diabetes for a long time will damage the nerves in your legs. Damaged nerves lead to a reduction or loss of sensation in the feet. So, if you wound your leg in any way, you might not feel it until it’s too late.
To make things more complicated, wounds tend to heal slower in people with diabetes since blood vessels can’t properly deliver blood.
All of these together can lead to a foot ulcer – an open non-healing foot wound. And, if an ulcer is not treated in time, it can become infected. There is also the risk of the infection spreading to the bone, leaving foot amputation as the sole treatment option.
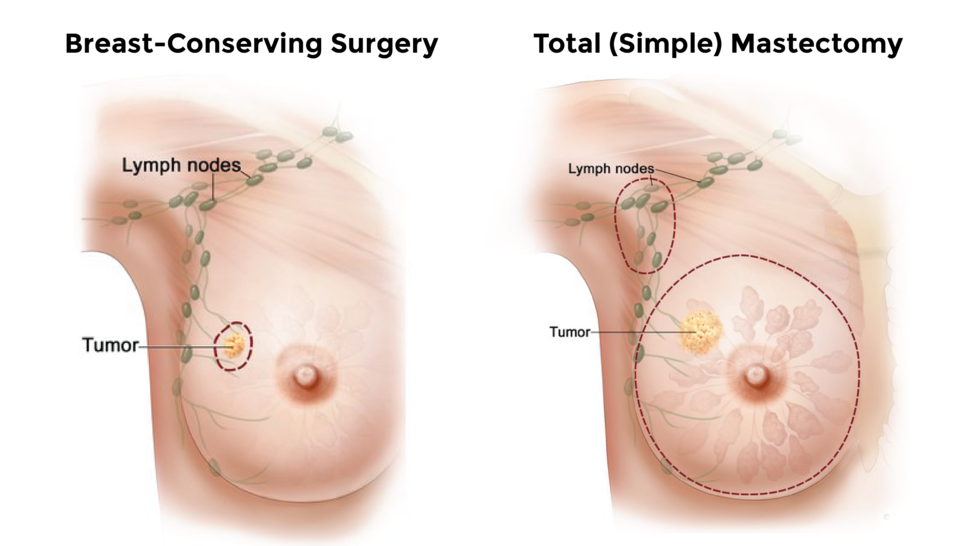
A breast lump is a mass that develops in your breast. While a breast lump can be a sign of breast cancer, often it is not related to cancer. Eight out of 10 breast lumps are noncancerous. If you feel a lump in your breast or under your arm, see your healthcare provider. Your healthcare provider will figure out the cause of the breast lump and determine whether or not it needs additional workup or treatment.
What does a breast lump feel like?
A breast lump may feel like a frozen pea or lima bean. It might feel hard or different from the rest of your breast tissue.
Does a breast lump mean I have cancer?
Breast lumps are one of the symptoms of breast cancer. However, often, breast lumps are not cancerous. Several other conditions can cause breast lumps.
Talk to your healthcare provider if you notice a breast lump. If it is cancer, treatment is more successful when started early.
Carcinoma of breast mean?
A condition in which abnormal cells are found in the tissues of the breast. There are 2 types of breast carcinoma in situ: ductal carcinoma in situ (DCIS) and Paget disease of the nipple. DCIS is a condition in which the abnormal cells are found in the lining of a breast duct.
Breast cancer is a disease in which cells in the breast grow out of control. There are different kinds of breast cancer. The kind of breast cancer depends on which cells in the breast turn into cancer.
Breast cancer can begin in different parts of the breast. A breast is made up of three main parts: lobules, ducts, and connective tissue. The lobules are the glands that produce milk. The ducts are tubes that carry milk to the nipple. The connective tissue (which consists of fibrous and fatty tissue) surrounds and holds everything together. Most breast cancers begin in the ducts or lobules.
Breast cancer can spread outside the breast through blood vessels and lymph vessels. When breast cancer spreads to other parts of the body, it is said to have metastasized.
The most common kinds of breast cancer are—
- Invasive ductal carcinoma. The cancer cells begin in the ducts and then grow outside the ducts into other parts of the breast tissue. Invasive cancer cells can also spread, or metastasize, to other parts of the body.
- Invasive lobular carcinoma. Cancer cells begin in the lobules and then spread from the lobules to the breast tissues that are close by. These invasive cancer cells can also spread to other parts of the body.
